Archives |
Historical Interviews of Retired Delaware CRNAsIn an effort to help preserve the history of our profession in the state of Delaware, DANA has decided to undertake a historical project of interviewing retired CRNAs.Willa Wing
I practiced as a staff RN for four years before applying to anesthesia school. As a graduate nurse, I worked on the infant floor at Mount Sinai Medical Center. At that time, Mount Sinai was in the process of creating a Pediatrics ICU and I became a core member of the first PICU staff. I worked in the PICU for almost two years and it was a learning experience. The ICU was a renovated large room within the infant floor that lacked space and had a poor physical layout. The medical and nursing care were fine but the work was stressful. Mount Sinai had a pediatric ER and I transferred there. During that time, I realized I needed to get out of staff nursing. I thought I’d go into public health and applied for a master’s program in public health at Columbia University. I went for an interview, got into a rather heated discussion about the goals of public health service with my interviewer (I only remember he said something along the lines of “A public health administrator is like a master puppeteer pulling the strings” and I thought he was the most arrogant and controlling person I’d ever encountered. That interview made me rethink my career choice. Needless to say, I didn’t get into public health school. So I was back at square one and I had to figure out what I was good at and what I enjoyed doing and that turned out to be critical care nursing. This is when I learned about nurse anesthetists and I started applying to anesthesia schools. I had little savings and I didn’t want the burden of any more school debt. I applied to three schools: two in the Philadelphia area (Lankenau and Nazareth) and one in Wilmington. All were certificate programs at the time. I got into Wilmington. Certificate nursing anesthesia programs were models of paternalism, in the more positive aspects of the word. They were benevolent but a strong sense of their notion of what should be taught influenced the education curriculum. For instance, my program did not teach the students how to perform any type of regional anesthesia—that was strictly the realm of the anesthesiologists. It was an autocratic system but you felt taken care of and protected, especially if you were a naif entering the program as I was. There was no tuition and every student received a small stipend. In 1982, it was about $350 a month which helped a lot with living expenses while you were attending school. I trained at the now defunct Wilmington Medical Center School of Anesthesia. I was a member of the next to last graduating class. Unbeknownst to me, it would prove to be a program that offered a strong foundation in forging clinical skills (with the notable exception of performing regional blocks.) When I applied to the school, a Bachelor’s degree (not necessarily a BSN) was a prerequisite. The other requirement was experience in an ICU or ER setting; OR experience was not necessary. (I remember that emphasis from the brochure.) Three different campuses, known as “divisions” comprised the Wilmington Medical Center: the General division, which was a women’s health hospital and included OB services, GYN surgeries and cancer care; the Memorial division, which had most of ENT and head and neck cancer surgeries, orthopedics, dental and OFMS, urology and some general surgery and the Delaware division. The Delaware division was where the Emergency Department was located so the “Delaware” was where you saw trauma cases, general surgery, neurosurgery, plastic, ophthalmology and non-open heart CV surgeries. (There was no open heart surgery in Delaware at the time I trained and consequently I’ve never had any experience of giving anesthesia for open heart cases.) The major ICUs were located at the Delaware division. The anesthesia school was located at the Delaware as well. There was some overlap in services between the Memorial and Delaware divisions but each division had its own, financially independent anesthesia department, with its own policies and distinct work culture. As a student, you had to be cognizant to not insult one department’s anesthesia staff by comparing clinical routines of how one division operated compared with another. It was “Anesthesia Diplomacy 101” and my fellow students (in the class above me as well as my own class) shared stories of experiences learned the hard way and offered each other sage advice on how to avoid stepping on the toes of your clinical instructors. The quality of the academics was directly related to the talents and knowledge of the instructor of the course. The instructors were all staff anesthesiologists or anesthetists who wished to teach a particular subject. My strongest instructors were in Basic Principles of Anesthesia (Dr. Aikens and Gerri Damiecki), Pharmacology (John Strange), Renal (Donna Minner), Cardiovascular (Drs. Hindin and Kittle) and Anesthesia Equipment Knowledge (Dr.Skinner). My weakest subjects were Pulmonary (Dr.Henderson) and Endocrinology (Dr. Abello). If you didn’t understand something in the classroom, you’d had to do a lot of independent reading. Fortunately for me, the first edition of Miller’s Anesthesia (2 volume set) was available in 1982 and Stoelting’s Anesthesia and Co-Existing Diseases was published in 1983. In the recent decluttering of my home, I found all my textbooks from my anesthesia school days. I trained in the analogue age. The anesthesia machines were primitive (see John Strange’s detailed descriptions) but were easy to troubleshoot. As an anesthesia student, you got to the workroom early to secure an ETCO2 monitor and a side arm mechanical ventilator (not all anesthesia machines had ventilators). If you couldn’t get a ventilator, you’d be hand-bagging a patient throughout the entire case. Imagine hand-bagging through an entire open AAA repair! (As a testament to this, my thumbs are arthritic and I have recently had steroid injections in both thumb joints.) The end tidal machine sat on its own spinal table and the (non-disposable) part that attached to the endotracheal tube was so heavy that dislodging the ETT was a real possibility and required much taping and vigilance. The rubber circuit hoses were so heavy that those tube holders or “Christmas trees” were an absolute necessity in those days (the weight of dragging rubber hoses could easily inadvertently extubate your patient.) I believe it took the AIDS crisis to finally get rid of the reusable rubber hoses and switch over to disposable kits. The kit consisted of a circuit, 3L bag and a CLEAR mask, all lightweight and disposable! Initially, there were no airway filters (HEPA or otherwise) attached to the circuit. During my senior year, the anesthesia department acquired pulse oximetry. This was a game changer and in my opinion, heralded the start of digital technology in anesthesia. Before, we were taught to look for circum-oral duskiness if we had trouble ventilating. Now we realized that the O2 Sat was probably in the 50s or 60’s by the time cyanosis was noticeable. With the pulse oximeter, intervention measures were much quicker. That tone modulation that occurs with decreasing saturation values was the best early alert system (and still is.) Many of the older surgeons were trained to be audibly aware (EKG beats, etc). I remember one particular surgeon would absolutely stop operating and look at me whenever the tone of the pulse oximeter changed. Shortly after its introduction, pulse oximetry monitoring became a standard of anesthesia care. Senior year in anesthesia school was also the first appearance in the department of the Drager Narkomed 2A machines. It was a Cadillac among the machines we had back then. I believe Dr. Hindin and Dr. Kittle (newbies in the department in 1982) were largely responsible for their purchase. It was still an analogue machine but it had an attached ventilator, scavenger system and a large workspace and shelves to put monitors on instead of creating an anesthesia circle of machine and multiple individual monitors on spinal tables (and don’t forget the anesthesia cart) surrounding the head of the bed. Think of Conestoga covered wagons encircling the patient in a very fortress-like manner. Having the Drager Narkomed was like going from a 1930s farm kitchen to a modern kitchen with space saving modular systems. However, habits formed early die hard. To this day, I am still territorial about my anesthesia “space” and will move cautery machines and endoscopic monitor towers away from “my space” when at all possible. Back to my education, which was closer to an apprenticeship in many ways. We received didactic teaching in the first month or two and then we were assigned with nurse anesthetists in the OR. There were a lot of mask cases in those days and our goal was to acquire and hone ventilation skills while slowly learning the surgical cases and how to give anesthesia. There was a lot of “hands on” education in a literal sense. You looked at your patient, you touched their torso area to see if the skin was warm and dry or clammy. (No Bair huggers in those days.) You checked their eyes: tearing was a sign of light anesthesia levels. You had an earpiece and were literally connected to the patient by a precordial stethoscope. It was the pre-digital age of monitoring. By the third month, we were intubating and doing longer cases (with the anesthetists) and given more responsibility. By the sixth month mark, we were rotating to the different campuses. If we were doing well, by the senior year we would be running our own OR rooms with anesthesiologists supervising (not necessarily in the room and depending on your attending, not always physically present during the case). We began taking overnight call sometime in the senior year. Call was a 16 hour shift on weekdays and 24 hours on weekends. It was understood that we would run our own ORs on call if the case was appropriate. The normal procedure for floor intubations was an awake, blind nasal intubation with minimal sedation. (That was always stressful for me.) The anesthesiologists took call from home while the CRNA and SRNA were in house. Though there was no tuition for our training there was a bit of labor exploitation, especially during the senior year of the program. Our anesthesia program reminded me of the hospital/certificate nursing school programs that were prolific throughout the country until the1970s. Student nurses learned during the day and as they advanced through the program, student nurses ran the wards at night. I came away from my anesthesia program with a confident set of skills. Taking call was when I learned to stop being timid and found my voice to express concerns with the surgical team. Taking call and doing floor intubations were when I learned to delegate and take control in Out of OR situations when I was considered “the airway expert.” (Expertise is all relative; I never hesitated to ask for back up when necessary.) The OR culture was different then. Experienced OR nurses stood next to you during induction (because you did inductions most of the time without anesthesiologists being present) and they knew how to assist you throughout the case if you needed help. An experienced OR nurse is a valuable team member. Surgeons are surgeons. One surgeon told me that he was “the Captain of the ship.” My attending anesthesiologist quickly disavowed that fact and told that surgeon that if he considered himself in control of “the crew”, he was also responsible (and liable) for any anesthesia complications. It’s always helpful when anesthesiologists have your back. That point was clear and well known, particularly at the Delaware division. The surgeons there were less likely to harangue the anesthesia students and anesthetists. I don’t find that level of support within our anesthesia department anymore. It’s more of an individual trait rather than a department banding together to stop any inkling of harassment by others in the operating theater or procedure rooms. In fact, in the years leading up to my retirement, there was a greater chance of my being “thrown under the bus” rather than an anesthesia colleague standing up to bullying in the OR. You need a thick skin in this profession. Nowadays, I think there’s a lack of appreciation of the skill set needed to perform a good anesthetic. Being an excellent anesthetist goes beyond knowing your algorithms and doing check lists. We all start that way but if you can’t go beyond that stage and you don’t develop empathy, a rapport with patients and a certain anesthesia “instinct” in your practice, you may as well just have an Anesthesia for Dummies book on your work table. What do I like most about being a CRNA? I enjoy meeting the patients and setting them at ease, whenever possible. I enjoy the patient interaction and I love it when a person emerges feeling comfortable and realizing that the procedure is over and they are recovering. I am also very proud of working with Dr. Steve Katz and Marianne Murch (the head of the anesthesia techs) as part of the core group that launched the first surgery center in the state of Delaware in 1993. At the outset, there was a dedicated anesthesia staff at the Christiana Surgicenter to ensure efficiency. There was no template to work with and no previous experience or available data on work flow for day surgery cases or MAC anesthesia policies, etc. But there was a lot of brain storming and thinking outside of the box and creative ideas from all staff members. Policies and guidelines were created and reviewed as the need arose. The place was an overwhelming success from its opening day and one of the reasons for its continued success is its ability to be flexible and meet the changing needs of the CCHS community. The following is my impression of the anesthesiologist-anesthetic dynamic as I experienced it. I often feel that in medicine, anesthesiology is a specialty that attracts people who like the research-able, scientific, measurable methodology aspects of the field. Certainly, the early anesthesiologists were also inventors and innovators who created a lot of equipment as the need arose. (I’m thinking of RAE tubes, MAC blades, various instruments for difficult intubations and more recently, LMAs.) The anesthesiologists who were my early instructors struck me as the more biochemistry, science minded, engineers of the medical world. The nurse anesthetists brought their critical care experience with them. They brought their knowledge of psychology and sociology and their listening skills as well as their managerial ability to prioritize (as well as a healthy dose of common sense.) It was a good match and made for a solid working team. That was then. Nowadays, I don’t think there’s much difference between the backgrounds and training of anesthesiologists and anesthetists anymore. The younger anesthesiologists are more down to earth and less paternalistic. I’m not at all sure what draws the younger generation of medical students to become anesthesiologists nowadays. The times have changed and the profession has evolved dramatically in my career lifetime. I often tell the new CRNAs and SRNAs that I don’t think I would succeed in an anesthesia program today. The leaps in knowledge in biology and biochemistry as well as all the technological advances in the past three decades would render me a remedial pupil in today’s programs. We work in a digital world now, which is so much safer for patient care. I am not as book smart or computer savvy as the younger anesthetists and SRNAs. I am very impressed with their intelligence and academic knowledge. Also, with today’s graduate school expenses (and growing PhD requirements for anesthetists), I’m pretty certain that I would not have chosen this career path under present circumstances. My first job at Sloan-Kettering in 1984 paid $37,500 (an envious sum when I graduated; but I earned every penny of that salary. Sloan-Kettering’s average turnover time for anesthetists was two years.) When I returned to Wilmington in 1986, I took a salary cut and my base salary was $29,500. Salaries improved within the next few years when the closure of the majority of certificate anesthesia school programs across the country created a shortage of available nurse anesthetists. Most of us back in that era didn’t enroll in anesthesia programs for the money. When I trained, the CRNA salaries were only slightly higher than ICU or ER nursing salaries. For me, I had to find something different than staff nursing or I was going to burn out. As an anesthetist, I never had the career frustration I experienced as an RN. The patient experiences that stick with me are the sad ones. I once had a 15-year-old boy who was a passenger in a motor vehicle accident. He was awake and alert and I was getting ready to put him under for an exploratory laparotomy. That boy was sweet and sassy and right before induction, thanked everyone in the room for taking care of him. Unfortunately, that child tore his vena cava from the impact of the accident and died after several hours of surgery and different teams working frantically on him. I will never forget his demeanor as he was being induced, just confident that all would be well. It was a very humbling experience and I went home and cried. That was at least twenty years ago and I remember it as clearly today as when it occurred. (My attending anesthesiologist for that case remembers it too, after all these years.) “You can learn something from everyone: from patients to senior staff members.” That is what Dave McKeever, CRNA (who was in the class ahead of me) told me. One of the anesthetists during my training was in her mid-60s (Ms. Zeebrook) and months from retiring. She LOVED using halothane as an anesthetic agent. “Well,” she told me, “if you’d spent the majority of your anesthesia career using ether (flammable) or cyclopropane (explosive), you’d think Halothane was the best thing since sliced bread, too!” When she said that, I totally understood where she was coming from. I didn’t care for her anesthesia but I got her perspective and respected it. For the SRNAs and new CRNAs, I would say keep up to date on the research and the new technologies in the anesthesia field. In the course of your career and as you gain experience, you will quickly figure out what is advantageous for the patient and what is just “noise” and not worth pursuing in the long run. Not every trend becomes a standard of care. There are “fashions and fads” in surgical procedures and that is true in anesthesia as well. Be flexible in your thinking and the anesthesia methods you use. Don’t be dismissive. Don’t be arrogant. This line of work has a way of humbling you when you least expect it. It’s important to take care of your mental health as well as your physical well being. Wait the ten minutes for extra help when moving or positioning patients. Down the road decades later, your back, knees and shoulders will thank you. Take your vacation time and use it to relax. That’s what it’s there for; it’s a mental recharge. Dr. Tolpin used to tell me, “Treat each patient like he or she is your beloved grandparent and you’ll always be able to look at yourself in the mirror.” I’ll go further and say “Put your patients’ needs first and be their advocate while they’re in your care and you’ll always be able to face the patients and their families with a clear conscience.” Being able to sleep at night is priceless. Retirement is a new experience. I’m enjoying it very much so far. It is definitely something to aim for and it will be upon you sooner than you think, so plan accordingly. I have enjoyed my career very much. Do what you need to do for your own happiness. But wherever you go and whatever you do, don’t burn any bridges. Remember, you work to live and not the other way around. Joan AdamsI began anesthesia school in the era of see one, do one, teach one, graduating in 1971. I graduated from nursing school in 1963 and went to work in the Emergency department at Delaware Hospital. At that time, the Delaware was considered the "trauma" hospital even though there was not such a designation recognized or designated to hospitals. My first day in anesthesia at the Memorial Hospital was memorable. I attended a 30-minute class about the psychological support of a patient and then I went to the OR and did cystos the rest of the day. I knew that green was good but had no clue how to use an anesthesia machine with pop off valve or any knowledge of anesthetics. The previous day I was working in the Emergency department. I was proficient in starting IV's and ventilating with an ambu bag, maintaining an airway and functioning in high-tension situations. It was a good thing I was comfortable with that. I was a person who could adapt quickly and was very comfortable with creating order out of chaos. I learned very quickly that this work was going to require much more than flexibility. I knew I was there to put people to sleep, but what did that mean? What did it truly mean and how was I to know if the patient was at a sufficient level for surgery? I didn't want to give too much anesthesia. I asked the question and was directed to check for a lid reflex. That was comforting to me. There was a way to check if the patient was asleep. I had to start the case with a straight needle, attached to an extension tube and a 50cc syringe of Surital (barbiturate.) There was no IV, just the syringe. At the same time, I was charting, taking blood pressure, and making sure the patient was breathing and assisting when he was not breathing, which is difficult to learn using a pop off, as you know. I was settling in to this. I felt good. This anesthesia thing might be all right. Then I noticed that everyone was looking at me expectantly. Oh, I had to tell the surgeon to start. As soon as the surgeon rammed the urethroscope into the male patient, I knew that the sleep level was not sufficient and maybe the lid reflex did not mean so much after all. The patient's arms and legs were flexing! The patient was trying to get up and grab the hot poker that was hurting his special boy. Hmm. More of this Surital stuff? All day long, I went through this continuing nightmare. Only yesterday, I wasn't allowed to give IV drugs. Now I was giving a drug that I knew nothing about; maximum dose, side effects, cautions etc. Yesterday I had respect for my efficiency and knowledge. Today, I am an idiot and struggling to not hurt anyone and figure out how to do this job. At the end of the day, I met up with my bud from ER. We had embarked on this adventure together. It seemed we were the only ones left in the department. We had been relieving people so they could go home! She said, "Joanie what have we done?" I replied, "I don't know but I am bringing a change of underwear tomorrow. This is terrible." Truth be told, I really did not know what an anesthetist did every day. I embarked on this journey to anesthesia totally ignorant. Additionally, I did not know what I wanted to do when "I grew up." One thing I did know for sure after this first day, that if this was to be my daily reality, I didn't believe anesthesia was the job I wanted when I grew up. When I reflect on what we did and what we went through, it was plain awful. I was confronted with stuff that could scare the bejesus out of you but there was no choice. I could not run away. I had to stay there and deal with the problem. Anesthesia was very primitive when compared with today. There were no monitors, no fancy machines, and no ventilators. You had a stethoscope, blood pressure cuff and a very few drugs. There was lots of exhausting nerve-wracking work. Today the anesthesiologists are involved in the care. In those days, you were on your own and it was understood that you should not be a nuisance and ask for consultation or help with a case. There was no evacuation system for waste gases, so you spent the day half anesthetized yourself. You were wasted at the end of the day. You had used up all your adrenalin and all the waste gases just wiped you out. I dripped Venithine and ether for tonsils too. It gave you a sense of pride if you got a child off to sleep and awake with no troubles. When I dragged into the house after work, my husband would say, "Phew, you stink! Tonsils again today?" Why did the staff think that the perfect case to learn intubation was on a child with huge tonsils obscuring most of the airway? Could it have been that they could avoid doing tonsils by sending in the students? I learned the job of being an anesthetist. It was really scary and difficult, but sometimes you really did not know enough to be scared. A senior student taught you and maybe a little bit by an anesthesiologist. The "school was closed" at the Memorial and then my education resumed at the Delaware Hospital, which is now the Wilmington Hospital. It was a little better. Anesthesiologists took a more active role in the anesthetic but you still spent long periods alone. There was very little formal teaching. I recall learning about muscle relaxants during a case while I am trying to concentrate on the patient. The anesthesiologist made notes on his pant legs to explain the physiology of the motor end plate and the difference in the two classes of muscle relaxants. All of that wisdom walked out the door with him on his green scrubs. The catchy line he gave me to remember the difference between the two classes of muscle relaxants was, "If you are shot with a poison dart, you just fade away." Using the only nerve stimulator in the department, you could watch the fade with the muscle stimulation. There was one or maybe it was two ventilators in the department. Most cases were hand ventilated. Finally, I completed the program and applied for a job at one of the four hospitals in town. The chief quoted an hourly wage and I reacted in a way that is not recommended for job interviews. I laughed out loud and asked, "Are you serious? You are joking right?" I had some nerve but really, I was shocked. I had heard that this man was a real terror but really, what could scare me? I had just been through eighteen months of anesthesia school that was terrorizing, humiliating, exhausting, and dehumanizing. I told this "terrifying" anesthesiologist that I could not accept that salary because I was making more working part time 3-11 in the emergency department. He countered with he did not believe me. I countered that I did not care if he believed me or not because it was truth and he could easily verify the information. I was prepared to return to the emergency department. I even made the phone call to determine if there was a full time position available. The anesthesiologist called the next day to offer me a quarter more per hour. I took the job, not because I thought it was a fair price but only for the chance that I might make more money in the future than I would have in the emergency department. As a head nurse in that department, I had already maxed out my salary. My anesthesia career began. I was not truly happy with anesthesia. I was most gratified working with patients. There was little of that in anesthesia. Then as is true now, there was the constant push to work faster and do more cases in less time. I had to find a way to do the work to meet scheduling needs as well as my personal needs of feeling the satisfaction of providing something comforting and rewarding for the patient. I had to learn how to be meaningful and supportative in five minutes as well as doing charting, starting the IV, and planning for any emergent episode during the case. I truly was not happy for about six months. I considered leaving the field and returning to my first love, the Emergency Department. Gradually, I settled in and found a way to make myself happy in the task. The patient had faith in their surgeon but they had never met me. I had an important function and they were frightened. I learned to give them comfidence in me and a confidence that I would take very good care of them. In the process of this interaction, those ten minutes had a meaning for me also. There was unhappiness in the staff about our treatment. They just complained. I decided to do what I thought was best and do what I had always done. tackle the problem head on. I would listen to the complaints and proposed solutions and got the group to focus on solutions. That evening I would go home and type the letter to the Chief and presented it the next day to the nurse anesthetists for their signature. They were frightened to do something like that. My attitude was that complaining without action was useless. I convinced them to sign the documents and gradually things changed. They were all afraid of confrontation with the Chief. I wasn't. I wasn't a bully or confrontational. I was just doing what I had always done, when faced with a problem. I looked at the problem for what it was and looked for the possible solutions. I knew that much could not be changed immediately, but a little at a time, things could be improved. At one point in time, around the early eighty's, the malpractice insurance costs reached a crisis nationwide. Anesthesia was assessed the most dangerous of the medical specialties. Anesthesia really was not very safe. Technology and drug development helped to change things somewhat. However, more importantly, the community of anesthesiologists and anesthetists began a critical assessment of the current practice in the process of rendering patients insensible to pain for surgery. Guidelines for safe practice were identified and practiced. Safety checks that are now considered routine were not always a routine. It became routine to assess the airway and find ways to identify difficulty. This is routine today, but this was not always universally true. Anesthesiology went from the highest malpractice risk to the lowest as these practices and others became uniform throughout the country. Nurse anesthesia education changed, with emphasis on the didactic as well as practicum. Research became part of the practice. The nurse anesthesia programs became master's level as the professional nurse entered with a baccalaureate degree. Technology has invaded the operating room. Surgeons want to do different procedures, which require more knowledge of the physiological changes being caused by these surgical techniques. Technology for anesthesia use supports this surgical technology. The pulse oximeter, access to ventilators, instant information about breathing dynamics, end tidal CO2 waveforms and measurement, ability to measure arterial pressure, EKG, blood gases, monitor for level of consciousness is a part of our every day practice. It surely was not a part of my practice in the beginning years of my experience. I personally think the pulse oximeter was the most important instrument and then it was followed by the end tidal CO2 monitoring. When we first started using it, the numbers dropped so low, that we did not believe in the validity of the machine. We changed some things and realized that these machines were correct. Wow! Anesthesia is a constantly changing field. This requires constant self- directed study of changes and research being done in the field. It can be difficult to balance family life, the long hours, and the requirement to constantly study and improve your knowledge. It is a difficult profession. Some days you feel like you have been walking on the precipice of disaster all day long. All of your adrenalin is gone. However, at the same time, there is personal satisfaction in the knowledge that you have given your all to successfully bring a patient through the surgery. Anesthesia is a solitary practice but there is a community of solitary individuals who will willingly give you every assistance when the stuff is flying in the fan. They know what help is required. There is no need to ask. They have been there before and they want to help. I enjoyed the humor at the lunch table. Much of it was sick and a release from the tension that each person was experiencing in each room. You are unaware of tension because it is just a normal part of the day. It is Saturday Night Live at the lunch table and a perfect release. It is great to work with very smart, funny people who are self- directed to accomplish the mission. I was asked to share words of wisdom. I do not know that I have words of wisdom for new CRNA's. Your world is different from mine. I suspect your focus in life and work is different. A great percentage of your life is spent at work. As with any work, you must find a profession or the one thing that gives you satisfaction and happiness. You must find something that brings you a feeling of positive accomplishment. Daily, you need to feel you have made a difference in your small part of the world. Change will continue in the field. The true challenge is the mandate to protect the patient as we meet surgeon's needs, the drive of the schedule, and the push to be ever more efficient to improve the bottom line. You must remain the bulwark to protect the patient from these present and ever demanding forces. I was also asked how anesthesia changed me. I don't really think anesthesia changed the essence of me. The traits that are required to be an anethetist had always been present. as far as I am concerned. I always worked hard from childhood and expected to continue to do so. I already had a thick skin that started from childhood so angry surgeons or anesthesiologists were just the normal in a day of work either in the Emergency department or the operating room. Emergencies and chaos never bothered me. This was something to analyze quickly and find a way to fix things. I enjoy working with people but at the same time I don't mind being alone with my own work. I enjoy helping patients through a frightening time, to give them comfort and confidence that all will be well; that they won't be left alone. The assurance and knowledge that I would not leave them alone seemed to be so important. I had a good tolerance for long periods without sleep or rest. I had the patience required to teach others how to give anesthesia. I was given the problem students to determine if they were trying to move in to a facet of work for which they were unsuited. I had the patience to deal with this and lead these students to realize on their own that this was not the field for them. They were so relieved when they were given permission to admit that which they sort of knew all the time. They were hopeful that this constant fear, nausea, trembling, and partial paralysis would pass. They had to come to the view that we all knew; they were not suited for this kind of work. Click here to download a document providing an overview of old anesthesia equipment. John Strange
I came into practice at an interesting time and saw a lot of innovations during my career. The following is my personal history. Feel free to edit it in any way that works for you. I always loved the sciences. I had my tonsils removed when I was 6 years old and kept them for years in a jar of formaldehyde on my bedroom shelf. I had a microscope and a dissection kit as a kid. We had a stream and a pond near our home where I would spend hours exploring the world of nature. My father was an orthopedic surgeon and I always loved his work stories. I had a keen interest in going into medicine and applied to medical school when I finished my undergraduate requirements. I was not accepted. I had received a BA in Biology from the University of Delaware and went to the university guidance center for advice. I was advised to look at through a bookshelf of graduate school catalogs and find a program that interested me (the university needed a more robust career guidance program for sure). I landed on a two year MS program in pharmacology at the University of Maryland at Baltimore. I learned very quickly that I had no interest in bench research. I liked the science but did not like working with animals that had to be sacrificed. I left the program after the first semester. From there I decided that I might be suited to teach high school science. After a short stint in teaching I found that although I enjoyed certain aspects of it I did not want to make a career out of it. It was after those two experiences that I decided to take more control of my career and enrolled in a five-week career guidance workshop. This particular workshop looked at your specific skills and talents and matched them to potential careers. After the five-week course I had zeroed in on a few career options that fit my skills and interests. The final stage of the workshop was to interview and spend a day with a practitioner in a profession of choice. On paper Occupational Therapist seemed like the perfect match. After spending a day with an OT I knew this was not to be the case. I like working with people and caring for them but the science was too soft for me. Another profession that was recommended was nurse anesthetist. I had never heard of the profession. I had however spent a month with my dad in his office and the OR when I was a senior in high school. I remember two things in particular. The first thing was talking to an anesthesia provider in the OR about how anesthesia worked. I was a reserved person at that point in my life and my dad was impressed that I was asking what he saw as an academic question. However, I was truly fascinated by anesthesia and wanted to know more about it. 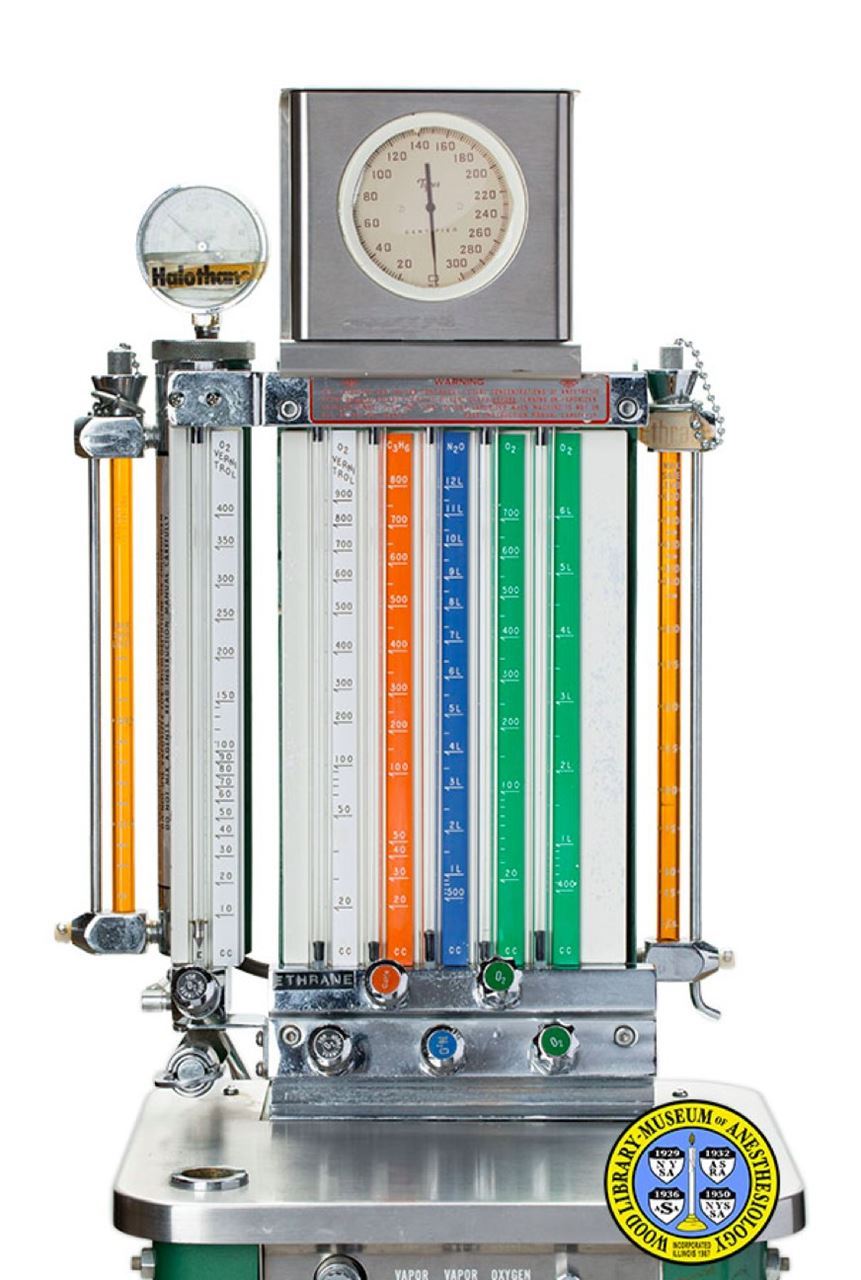
The other occurred when I went to the ED with my dad to watch him set a broken arm under anesthesia. I remember seeing the anesthesia machine and thinking it was one of the coolest things I had ever seen. The nobs, the flow meters, the colored tanks, the rebreathing bag, the green, blue, orange and white columns all fascinated me. I asked my father if he knew how to use the anesthesia machine (back then I naively thought doctors knew everything). He said he did not – that impressed me. To continue my career quest I spent the day with a nurse anesthetist. Her name was Donna Minner. She had an anesthesia student with her that day (Sue Leininger). Unbeknownst to me both of these women would become my colleagues and friends someday. The anesthesia machine had a “C3H6'' on one of the nobs. I had studied organic chemistry and recognized the formula and said – “cyclopropane?” – she said “yes – we don’t use it anymore but we used to use it as an anesthetic.” After spending the day with Donna and Sue and watching what the job entailed I was hooked! It was not only the hard science that appealed to me but also the whole package of working with living systems, patient care, responsibility, teamwork and independence. From that point (winter of 1976) it would take five years to do all the things needed to complete my anesthesia training. I had to complete a nursing degree, work in critical nursing for at least a year and then complete a two-year anesthesia-training program. My wife was a first year student at the University of Pennsylvania Veterinary School at the time and we were living in Philadelphia. I was able to enroll in the University of Pennsylvania’s School of Nursing and finished my degree in December of 1978. From there I worked at Hahnemann University’s coronary care unit (CCU) for two years. (My starting salary was $6.10 per hour). A lot was going on at Hahnemann Hospital as it was a large, university based research hospital. Some of the research involved a new drug class called calcium channel blockers. They were just being trialed nationwide and Hahnemann was one of the research centers. Many of the trails were done in the CCU. Also on the staff was Eldred Mundth MD who helped pioneer the intra aortic balloon pump. From my perspective it was a great job and it gave me the necessary experience to continue on to anesthesia training. In 1980 there were close to 200 certificate programs in nurse anesthesia. The times were changing however and Ira Gunn and the AANA had suggested that Nurse Anesthesia should move into the University setting and that a Masters Degree should become the entry level into the profession. This would be a slow process. In 1980 there were only two MSN programs in the country. My wife had been accepted to an internship in Veterinary Medicine at the Animal Medical Center in NYC. In addition to a few certificate programs I had applied to Columbia University’s program (MSN) and was accepted into their second class. That was where I decided to go to school to learn the art and science of anesthesia. The program was in its infancy in its transition from a certificate program at Roosevelt Hospital in Manhattan to an MSN program at Columbia University. Consequently, the entire anesthesia related classes were still taught at the hospital by CRNAs and MDAs. The courses required by the University to fulfill the MSN portion were taught at both the main campus at 120th street and at the Nursing School at 168th street. The program was “front loaded.” That meant that all the didactic courses were taught the first year and the second year was purely clinical. Our level of clinical experience was adequate for graduation but was much less than the experience that one received in most certificate programs. New York City offered many opportunities for clinical training and our program had affiliations with hospitals all over the city. To name a few – Neurosurgery - Columbia Presbyterian Hospital at 168th Street: Obstetrics - Maimonides Hospital Brooklyn: Open Heart – St. Luke’s Hospital: General Surgery - Roosevelt Hospital. I loved getting to know the different parts of the city by going to all the different institutions and to work with so many different practitioners. I also worked part time in the ICU at Roosevelt my first year. This was purportedly the oldest ICU in the country. The most memorable thing I did was care for a patient in an iron lung. I had never seen one before or since.
The Medical Center of Delaware came about after three hospitals came together in 1965. They were the Memorial: a general hospital, where they practiced urology, ENT and orthopedic surgery; the General: this was primarily an obstetrical hospital; and the Delaware (the “Big D”) which was the largest of the three hospitals where neurosurgery, large abdominal surgery, general surgery, pediatric surgery and the major traumatic emergencies came. There was also a neonatal ICU at the Delaware Hospital. When Christiana Hospital was opened in January of 1985 both the Memorial and the General were closed. The Delaware Hospital remained open and was renamed the Wilmington Hospital.
After only a few weeks of practice we took call. The MDAs went home when the day cases were done and the CRNAs stayed in the hospital. If there was an emergency case we called the MDA and they decided if they were to come in depending on the case. If there was an in-house intubation we were told to “do our best” but we were NOT to call them. The practice of the MDAs not coming in changed within my first few years. A younger group of docs had been employed and they started to come in for all cases. Eventually, they stayed in house with us. The OR coverage was organized such that every day the CRNAs were supervised 2/1 or 3/1. There was an MDA assigned to their own room almost every day. The docs really liked giving anesthesia and I remember coming on call one afternoon and when I went to relieve a doc he refused so he could finish the case!!! I am not sure how the finances worked out but that model is no longer being used. All patients were seen by a MDA. We usually started and ended our cases without supervision and only called if we felt we needed help during a case. There was a comfort level that the MDAs had that sometimes baffles the imagination today. I remember being on call one night and we ran three rooms simultaneously. I was in one room with my patient and the doc had two rooms to himself going back and forth between the two rooms through the connecting sterilization room taking care of the both patients! Another night a CRNA (Ralph Kochert) was given a dinner break by his supervising doc. He was in the cafeteria eating dinner when a few minutes later the doc sat down next to him with his dinner. Ralph asked who was watching the patient. The doc said the patient had been placed on the ventilator and the OR nurse was watching the patient. Ralph said he never ate his dinner so fast! All anesthesia equipment (hoses, face masks, stylets and airways) were cleaned and reused. We had all rubber hoses and face masks. They were stripped from the machines at the end of each case and placed in a special washing machine. I remember pressure checking a machine one day and found that it would not hold pressure because the hose was perforated with holes from overuse. Sodium thiopental (Sodium pentathol) was our main induction agent (we did also have methohexital and ketamine). All drugs were given by needle through an IV port. If we had a significant amount of induction agent left over from one patient we saved it and used it on the next patient. This practice stopped around 1983 when it was shown that HIV (HIV was discovered in the US in 1981) could be found in the IV tubing of infected patients and might contaminate the drug in the syringe. We had two ventilators for 8 operating rooms. They were of the “hanging bellows” type (yes the ones that you can’t tell if the bellows is actually delivering any tidal volume). It was “attached” to the machine with a pole that fits through a hole in the side of the machine. It was top heavy and unwieldy. If you had a case that justified the use of a ventilator you had to find one in one of the ORs and ask for permission to use it. Otherwise, all patients were ventilated by hand. When I retired in 2018 the old Ohio machine and ventilator were on “display” in the Wilmington Hospital anesthesia office. The anesthesia machines had E cylinders for both oxygen(2) and nitrous oxide(2) as they do today. That was our only source of compressed gas as there was no central piping. Consequently, we had to keep an eye on the levels of the tanks. We would switch them over in the middle of cases when needed and change them when they were empty. In 1983 the medical center decided to change vendors for the compressed gas tanks in order to save money. A green tank marked “oxygen” was taken out of the storage room by a student nurse anesthetist named Willa Wing. When she changed her tank and opened the valve she noticed the pressure went to 750 psi not the expected 2000 psi. Astutely, she perceived something was amiss and removed the tank and brought it to her preceptors attention (Sue Leininger). After removing the tank they could see that although the pin index holes were correct for oxygen the company had somehow managed to force the nitrous oxide into the tank. One could see the marks on the tank where there had been compromise to the index system. This speaks to why one does not always hire the lowest bidder. After that incident the medical center went back to the more expensive, more reliable company. Clearly, a major tragedy was avoided that day and future days! Most patients who were not intubated were managed by face mask as there were no LMA’s used in our practice until 1992. All laparoscopic cases were initially done with a face mask. This practice changed when one group of gynecologists insisted that all their patients be intubated. There was an article in the OB/GYN literature that described some bad outcomes (death) of patients having laparoscopies with facemask ventilation. Primarily, it was obese patients being hypoventilated. Rather be selective with our patient population we went all in with intubation. I know I was one of the few who would do laparoscopies with a mask (LMA in this case) up until I retired. If a patient met three criteria and my supervising doc was on board (criteria number 4) I would use an LMA. The criteria were: virgin belly (no previous abdominal surgery), acceptable BMI, and relatively quick surgeon. Despite training students that using an LMA and a muscle relaxant is acceptable practice I could not convince many to adopt the practice. I suppose because we did so many hand ventilated mask cases and would use muscle relaxants (mostly succinylcholine drips) I had a comfort level and experience that others did not have. Some plastic surgeons like muscle relaxation for a short portion of their breast augmentations. I would use an LMA and give a small dose of rocuronium for that portion of the case. The patients would do fine and would most often not receive any reversal agent as they would be fully recovered by the end of the case. At the start of my practice we had just a few muscle relaxants: curare (D-tubocurine), metacurine, pancuronium and succinylcholine. As I said before for the shorter cases we used succinylcholine drips. The number of muscle relaxants expanded in the 1990s and has since contracted to just a few choices. On the whole they are more forgiving as compared with curare and pancuronium which lasted for a long time and could be hard to reverse compared with the intermediate acting drugs of today. When I was a student nurse anesthetist the only two inhalation anesthetics in common use were halothane and enflurane. A new agent called isoflurane came into practice when I was in my second year of training. None of those agents are in use currently. We also used nitrous oxide in most cases.
Using the whiz wheel:
Although it was not possible to give a hypoxic mixture with our machines I do remember one of the machines having a nitrous oxide flush valve where you could give 100% nitrous oxide when it was pushed. All blood pressure was taken manually. The operating tables were all manual. You would “pump” the table up with a food pump. We had gears and a rotating arm on the side of the table for putting the table in Trendelenburg or reverse Trendelenburg as well as for raising and lowering the lower half of the bed.
When the surgeon made an incision we would watch and make a notation of the blood color and flow. If you look at old anesthesia records you will often see BRBB notated at the time of incision. This stood for “Bright Red Brisk Bleeding”. It was felt that the color of the blood and the briskness of the flow showed both adequate oxygenation and adequate blood pressure. We discovered when pulse oximetry became available that even though the blood looked dark in the surgical field it did not mean that the patient was not being well oxygenated. Before the common use of pulse oximetry the surgeon would remark if he or she thought the blood looked dark during a procedure. It was very important to assess if the patient was being adequately ventilated when this was shared by the surgeon. We had a tragic case that resulted in a patient ending up in an unrecoverable coma for years. The surgeon had mentioned repeatedly that the patient’s blood was dark but was ignored by not one but two anesthesia providers. After years of litigation they were both not allowed to practice anesthesia. Pulse oximetry and end tidal carbon dioxide monitoring of course changed our practice tremendously. It has made anesthesia much safer and has brought down the cost of malpractice insurance.
A “neo-wash” was another method of administering a sympathomimetic that was abandoned in the 1980s. It involved drawing up an amp of phenylephrine into a 3cc syringe and then returning the drug back to the ampule. After that 3ccs of sterile saline was drawn up into the syringe, rotated a few times to mix the drug with the saline and then injected into the patient's IV tubing. Unfortunately, you did not know if you were giving 50 or 300 micrograms of phenylephrine so the technique was abandoned for more precise methods of administering phenylephrine. Intubations were often very challenging. We had both straight and curved blades available but no fiber optic options. There were many, many types of blades - all variations on the curved and straight blade theme. I remember sometimes taking over an hour trying to intubate a patient. We would continue to hand ventilate while various practitioners would come in and try their favorite blade but sometimes to no avail. Consequently, some cases would be cancelled due to inability to intubate. I remember one case where the patient was a very difficult intubation. It was not my case but ended up being presented in one of our monthly M and M conferences. We had a very skilled surgeon who was always on time and anxious to get started as he had a very busy practice. He was often gowned and gloved while we were inducing the patient. The day of this difficult intubation he was watching the struggle and announced that the patient had not come to the hospital for anesthesia but had come to have her gallbladder removed. He was able to convince the anesthesia team that he would be able to remove that gallbladder if they would forgo the intubation and “face mask” the patient. He could be very convincing and they agreed. The gallbladder was removed without complications. Despite the positive outcome this was not received well by many of the members of the anesthesia department. It was felt that surgeons should not be dictating our practice by most at the conference. It is of course always easy when you're not in the trenches to make these pronouncements. Floor intubations were mostly done nasally with the patient spontaneously breathing. We became quite skilled at these intubations. We would place our ear near the end of the ET tube and move the patient’s head and neck in all directions in order to line the ET tube up properly to intubate the trachea. When everything seemed right we would advance the tube. This practice went on for many years until it was shown that there was an increase in pulmonary infections from nasal pharyngeal contamination of the ET tube. Generally speaking I loved the job. I really liked it when it felt like you were working as a team with all involved in a common goal. When I started out it was not uncommon for surgeons to throw instruments and carry on. I remember hearing one reformed surgeon say that he threw instruments because he did not think people were there to help him. Once he realized that everyone there was there to help he stopped acting out. I know there continues to be surgeons who act out for whatever reason but I have always told myself when that happens that they just haven't realized that everyone is there to help them. Students and teaching: At the time of my employment in November of 1982 there was a two year certificate program at the Medical Center of Delaware.This was the standard length of time for most certificate programs although there were a few exceptions. All non masters degree programs paid the students a stipend in their second year. The program was run by our chief nurse anesthetist Geraldine A. Damiecki (later Geraldine Irish) and Gerald J. Savage, MD. It was a strong program that trained some of the best CRNA’s that I have ever worked with. I asked to teach the pharmacology class to the second year students and was granted permission. I had a passion for pharmacology, especially, the autonomic nervous system. I had taken an exam writing course at Columbia University. It was a great course and allowed me to write excellent questions for our students that were even used in the certifying exam for the AANA. Sadly, the program closed in 1986. This was due to two major factors: first, was the move from certificate programs to masters degree programs and second, was the opening of Christiana Hospital which required a great deal of energy and focus as three hospitals were being consolidated into two with all the different anesthesia groups coming together under one roof. I will digress from the school and teaching for a moment. The consolidation of the anesthesia groups did not go well and it took many years for it to settle out. There was a discrepancy in board certification amongst the members. Many of the MDAs from the General and Memorial had trained in other countries and immigrated to the United States but were not board certified. Some had trained in the US but had never received board certification. The Delaware Hospital group were all board certified. Each department had a chairman before the consolidation. They all had strong egos. How to share chairmanship, work load, and compensation became a major issue with much infighting and division. The non board certified members were relegated to the lower compensated positions. The chairmanships were shared on a one year rotation basis. This caused great tension. At one point I was even asked to be part of an anesthesia group as a partner but that never panned out. It did eventually get worked out but was very dramatic with all the elements of a congressional showdown. Back to the school and teaching. A few years after the school closed it became apparent that we needed to continue to train local talent that would stay and work in the community. Consequently, we affiliated with a program at the Medical College of Pennsylvania that was run by Mr. Michael J. Booth and Dr. Athole McNeil Jacobi. We started with two students and I was the clinical coordinator. My job was to make sure the students received the clinical training necessary to sit for the board exams upon graduation. We had a great clinical site that provided everything the students needed except their pediatric training which they received at the A.I. duPont Institute. What made our institution a great place for their training was the large volume of cases, excellent clinical instructors and the lack of competition for cases by other training programs. The program grew over time and moved through three universities. After being moved to Hahnemann University for a few years it finally ended up at Drexel University. The program started with about 10 students and we helped train two or three students a year at Christiana Care. It has evolved to a class of over 25 students with 10 being trained at our institution today. I worked in the position of clinical coordinator for 10 years. In 2002 I thought I would try my hand as a professor and took a position of Assistant Professor at Drexel University’s nurse anesthesia program. For me it was a great opportunity to review and relearn so much of what I had forgotten. As a student you tend to study everything as you don’t know what is important. But after twenty years of practice you can distill what you know is important for practice and then share it with students. I will say that certain aspects of teaching I enjoyed a great deal. However, I was not cut out to be a university professor and returned to clinical practice and clinical teaching which I enjoyed tremendously. I loved the variety and challenge of the job. I even enjoyed being on call and being up all hours of the night both in the general OR and OB. Being on call did have it’s negative effects. It was difficult at times with my wife having her own career and us also having two children to raise. And, as those who take call know, it can be very physically demanding. It did become very hard for me to sustain being on call when I reached my late fifties. At that point I did not think it was really in the best interest of the patients I cared for to take call, and so I stopped. One of the great things about being a CRNA is that one can work part time so one can “ease” into retirement. Over the final six years of practice I gradually reduced my schedule to two twelve hours days a week. This was very helpful as it allowed me to get a feel for retirement and for my wife to get used to having me around the house. I was looking forward to retirement but when it got close I started to feel regretful mostly because I knew I would miss working with so many wonderful people. Our daughter, Abby, has become a CRNA and is working in Saint Louis, Missouri. I asked her to look over this document for her comments. She noticed I did not share any advice to new students. I told her I really did not know what to say but I have given it some thought. I think one of the most important things I learned over the years is that “less is more.” We tend to over medicate on so many levels especially narcotics and muscle relaxants. But also we often reach for a sedative or hypnotic when more often what is needed is our learned skills of calm reassurance. Mixed with humor if possible can also help if appropriate. Best of luck to all who venture into what another colleague, Dave McKeever, correctly said so many times is “the greatest job in the world.” Gerri Irish
How many years did you practice as a CRNA?

Well- it has become a job only such that all CRNAs are not dedicated to the profession. Not sure I get this question? What did you enjoy the most about being a CRNA?
Learn as much as you can from your peers and your mentors - no matter who they are and what profession they practice. Never stop learning…patients depend upon us for that! You make a good salary - save a portion of it so you can enjoy security later when you cannot work anymore. That day comes sooner than you think! Cheryl Richter, CRNA, MS
Where did you work?
Where did you train?
How did you train and what equipment did you train with?
Why did you become a CRNA?
Did you have any mentors coming into the profession?
What are the greatest changes in anesthesia practice you saw during your career?
What are the most significant changes you’ve seen in work culture?
What did you enjoy the most about being a CRNA?
Do you have a specific patient or experience that has stuck with you?
How do you feel that being a CRNA has changed you as a person?
What are you looking forward to (or are currently enjoying) the most in retirement?
What words of wisdom would you give to a SRNA or new CRNA?
Maura Sheridan-Walther, CRNA BSN
My education in this nursing specialty commenced with the certificate program offered by the Medical Ctr of DE, under the direction of Gerald Savage, MD and Geraldine Damiecki, CRNA. We had a true weekly mix of didactic and clinical experience, even in the first months- moving seamlessly through theory and practice guided by nurse anesthetists and physicians (no simulations for us!) A hair raising real-time application of our new found skills was made possible by those CRNA instructors, physicians, and adjunct personnel who expected us to function as competent members of the operative team. Our mentors, the clinical instructors, led by example. We worked with Vernitrol vaporizers, Draeger machines being state -of-the-art. Pediatric training included Mapleson, then Bain circuits. Red rubber endotracheal tubes, non-disposable circuits, and heavy non-disposable masks in several different styles to fit certain anatomies prevailed. Truly cumbersome arterial line and cardiac output set-ups required seemingly constant adjusting. Penthrane, Halothane, Enflurane, and wonder of wonders- Isoflurane were in use. Iso came on the scene with a lot of complaining about it’s irritating pungency, much to our chagrin as we breathed down infants/children. Pentothal was THE hypnotic; no one excited by etomidate, Propofol light years away. Metubine, D-tubocurare, Gallamine, Succinylcholine, and Pancuronium- that’s all there was folks! Want to expand plasma volume? That was left to Albumin, or blood products until Hetatstarch appeared. “Blind” intubating techniques were feared and admired - certain techniques to be prized like Heisman trophies. The biggest and best changes I saw during my career included the pulse oximeter, the video laryngoscopes, advances in fiberoptics, and the induction agent which changed the landscape- Propofol. Outpatient-friendly inhalation agents , pre-emptive analgesia, antiemetics, and judicious use of local/regional anesthetics upped the early discharge game. Methods and machines to avoid barotrauma, and simulate a more physiological lung amazed us. Computer driven charting did not totally amaze us, as more attention was diverted from the human being in front of us. Input finally fought to challenge output. Along with AI and digital recording, data is driving the bus now. We were supporting life, but sometimes in the darkness of not having complete information. Clinical simulation and best practice guidelines will hopefully “lift all boats” evening out individual differences in breadth of clinical experience. It will take exceptional skill to bridge the gap between human and artificial intelligence. With fewer practitioners, the challenge will be to administer anesthesia more efficiently, in both time and accuracy of consistent safe endpoints. My hope is that the humanity of it all will not be lost. As you might suspect, for me, the most enjoyable part of the profession WAS the ever-changing landscape of technology and technique that so improved a patient’s experience. The icing on the cake though was the chance to creatively apply these things in an artful manner that would lead to a superior outcome. This required an intuitive understanding of the person in front of you combined with a broad-based skill set: deep understanding of anatomy, physiology, microbiology, pharmaceutics, chemistry, and physics….not to mention a dash of psychology and machine engineering. The profession changed me, as one might expect in several ways, though you could argue that most good anesthetists embody these characteristics , even if undiscovered prior to entering their formal education: hypervigilance, attention to detail while concomitantly seeing the big picture, rapid assessment of any given situation followed by an action plan, and organization. On-call nights sleeping next to preserved brains-in-a-jar had to be THE most bizarre out of OR experience ever. I have never asked another CRNA if they remember more good cases, or is it the untoward outcomes that float to the surface? In our efforts to control outcomes, the great ones have always landed in the high “good” pile, while the undesirable outcomes continue to dog us for years. It takes strength and courage to move past the root causes and internal reviews over three plus decades of practice. I fear that independent thought and creative application of the sciences/technology to a particular patient will be lost in the relentless drive to match data to ALL outcomes. The trend was in that direction as I retired. A message to CRNA’s: let your voices be heard. Continue to involve yourselves in patient- centric and quality control initiatives. Champion safety research. Continue to educate yourself and share knowledge with your peers enthusiastically. It almost seems trivial to mention how life has turned in another direction upon retirement. We/you can always reinvent yourself-- look at George Plimpton (cultural reference- Google it!) I look toward peaceful balance, in body and relationships; seeking unknown and interesting “rabbit holes”. Most days I drive to work through a preserved acreage of ponds, flowing creeks, wildlife, and incredible outdoor design- all mixed with a deeply curated display featuring decades of interiors of people’s lives. Stay inspired , all you who travel this path. Minori Thorpe.JPG) How many years did you practice as a CRNA? How many years did you practice as a CRNA?
|

 I recently retired as a nurse anesthetist, having passed me exams for certification 37 years earlier (in 1984). Essentially, I have only worked at two places: Memorial Sloan Kettering Cancer Center (MSKCC) in New York City and Christiana Care Health Services (CCHS). I have worked with CCHS since 1986. I moved here because I wanted to start a family (my biological clock was ticking) and NYC housing and child care costs were out of my league.
I recently retired as a nurse anesthetist, having passed me exams for certification 37 years earlier (in 1984). Essentially, I have only worked at two places: Memorial Sloan Kettering Cancer Center (MSKCC) in New York City and Christiana Care Health Services (CCHS). I have worked with CCHS since 1986. I moved here because I wanted to start a family (my biological clock was ticking) and NYC housing and child care costs were out of my league. I’m very appreciative for this opportunity to provide the DANA with my experiences in the wonderful world of anesthesia. This will also provide me with the opportunity to put in writing something for my kids and grandkids should they ever want to read about my life as a nurse anesthetist.
I’m very appreciative for this opportunity to provide the DANA with my experiences in the wonderful world of anesthesia. This will also provide me with the opportunity to put in writing something for my kids and grandkids should they ever want to read about my life as a nurse anesthetist. Upon graduation I secured a position at the Medical Center of Delaware (later to become Christiana Care Health Systems) as a staff nurse anesthetist. I was interested in working there in part because it had a certificate program and I had a keen interest in teaching pharmacology to the students as well as to do clinical teaching.
Upon graduation I secured a position at the Medical Center of Delaware (later to become Christiana Care Health Systems) as a staff nurse anesthetist. I was interested in working there in part because it had a certificate program and I had a keen interest in teaching pharmacology to the students as well as to do clinical teaching. I worked at the Delaware Hospital (starting salary was $12.50/hour). I did not go into the profession because of the salary (I was naive in my early 20’s thinking that money didn’t matter). However, the salary did start to take off in the 1980s. My salary doubled every ten years for the first 20 years ($25.00/ hour 1992 and $50.00/hour in 2002). Since then the salary leveled off.
I worked at the Delaware Hospital (starting salary was $12.50/hour). I did not go into the profession because of the salary (I was naive in my early 20’s thinking that money didn’t matter). However, the salary did start to take off in the 1980s. My salary doubled every ten years for the first 20 years ($25.00/ hour 1992 and $50.00/hour in 2002). Since then the salary leveled off.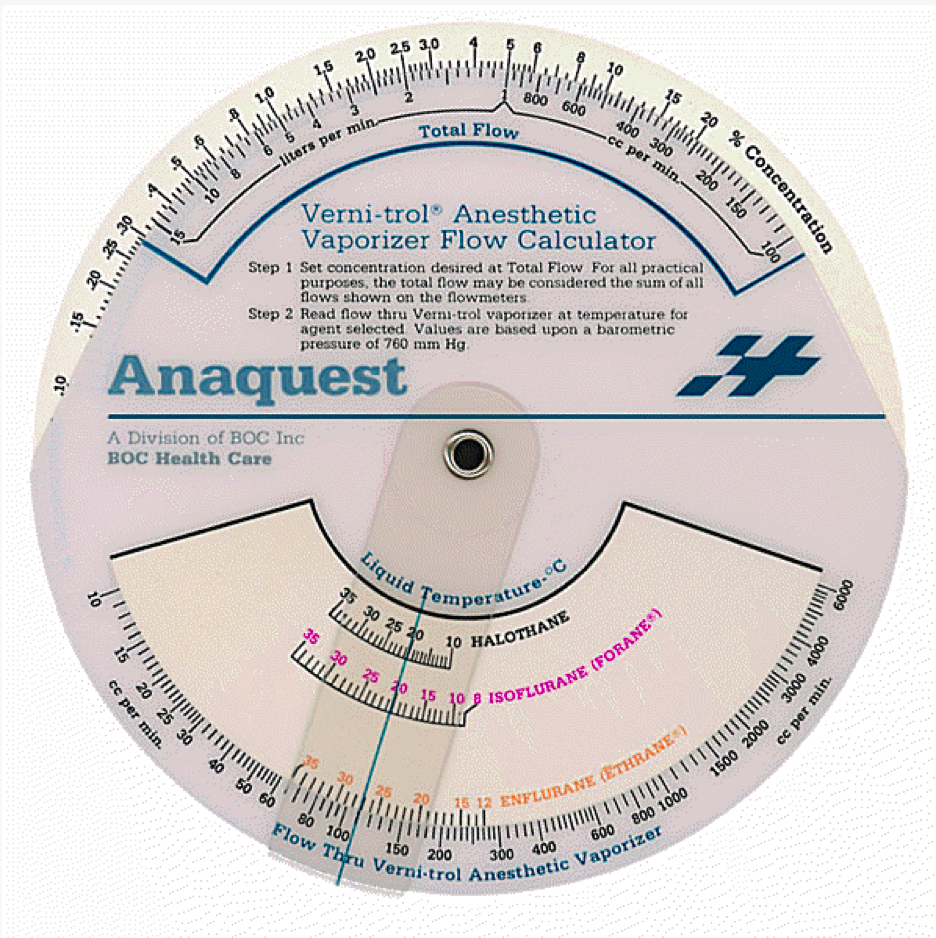 The vaporizers on our machines were not calibrated to give a certain percent like the modern machines. We had to switch that opened up the flow of gas through the vaporizer. We then regulated the amount of flow (and thus the concentration) with a nob.The switch when turned the other way would give you an oxygen flush. After flushing the system with oxygen which might have been necessary because the patient became hypoxic you might forget to return the switch to open the flow to the vaporizer position. The patient would let you know that you had only oxygen and nitrous oxide running when the surgeon made an incision, however. We had to calculate the percentage based on total gas flow, temperature, and the flow through the vaporizer. If your total gas flow doubled then the concentration was cut in half. If you doubled the flow through the vaporizer then the concentration changed based on the total gas flow. To do this accurately we had something attached to each machine called a whiz wheel.
The vaporizers on our machines were not calibrated to give a certain percent like the modern machines. We had to switch that opened up the flow of gas through the vaporizer. We then regulated the amount of flow (and thus the concentration) with a nob.The switch when turned the other way would give you an oxygen flush. After flushing the system with oxygen which might have been necessary because the patient became hypoxic you might forget to return the switch to open the flow to the vaporizer position. The patient would let you know that you had only oxygen and nitrous oxide running when the surgeon made an incision, however. We had to calculate the percentage based on total gas flow, temperature, and the flow through the vaporizer. If your total gas flow doubled then the concentration was cut in half. If you doubled the flow through the vaporizer then the concentration changed based on the total gas flow. To do this accurately we had something attached to each machine called a whiz wheel. We had no pulse oximetry or end tidal carbon dioxide monitoring when I started in practice.They were both introduced in 1985. We wore a precordial stethoscope that had a stopcock so we could listen to heart and breath sound and then we would rotate the stopcock to take the patient’s blood pressure and listen to Korotkoff sounds.
We had no pulse oximetry or end tidal carbon dioxide monitoring when I started in practice.They were both introduced in 1985. We wore a precordial stethoscope that had a stopcock so we could listen to heart and breath sound and then we would rotate the stopcock to take the patient’s blood pressure and listen to Korotkoff sounds. Drug drips especially sympathomimetics were administered without the benefit of infusion pumps or syringe pumps. We attached something called a dial-a-flow to the tubing to regulate the flow. They still existed in the workrooms of both Christiana Hospital and Wilmington Hospital when I retired although I don’t know of anyone using them except perhaps in the open heart area.
Drug drips especially sympathomimetics were administered without the benefit of infusion pumps or syringe pumps. We attached something called a dial-a-flow to the tubing to regulate the flow. They still existed in the workrooms of both Christiana Hospital and Wilmington Hospital when I retired although I don’t know of anyone using them except perhaps in the open heart area. How many years did you practice as a CRNA?
How many years did you practice as a CRNA? 1983-2016, spanned 33 years of practice as a CRNA, working continuously throughout those years for the various corporate entities that began with the Wilmington Medical Center, through Med Ctr of DE Inc., ending as Christiana Care Health Services. Had the pleasure of closing hospitals and operating rooms behind me as I pursued my career- from multi-specialty surgery, to OB/GYN, to ambulatory surgery; wrapping up the last 16 years as CRNA site director for the Roxana Cannon Arsht Surgery Center.
1983-2016, spanned 33 years of practice as a CRNA, working continuously throughout those years for the various corporate entities that began with the Wilmington Medical Center, through Med Ctr of DE Inc., ending as Christiana Care Health Services. Had the pleasure of closing hospitals and operating rooms behind me as I pursued my career- from multi-specialty surgery, to OB/GYN, to ambulatory surgery; wrapping up the last 16 years as CRNA site director for the Roxana Cannon Arsht Surgery Center.